What is Thalasseamia
GENERAL QUESTIONS
What is Thalassaemia?
Beta Thalassaemia is one of the most commonly inherited disorders in the country, with a prevalence rate of 6 % in the Pakistani population. There are more than 50,000 Thalassaemia patients registered with associations and treatment centers all over the country.
Thalassaemia associations in Pakistan have joined hands and formed a Federation by the name of Thalassaemia Federation of Pakistan
Treatment of Thalassaemia
Specific treatment for Beta Thalassaemia major will be determined by doctor based on:
- Age, overall health, and medical history
- Extent of the disease
- tolerance for specific medications, procedures, or therapies
- Expectations for the course of the disease
Patient’s opinion or preference
Treatment may include
- Regular blood transfusions
- Medications (to decrease the amount of iron in the body called iron chelation therapy)
- Splenectomy (surgical removal of the spleen, if necessary)
- Daily doses of folic acid
- Possible surgical removal of the gallbladder
- Regular checks of heart and liver function
- Genetic tests
Bone Marrow Transplant
Cure of β-thalassaemia can only currently be achieved by haemopoietic stem cell transplantation (HSCT), which includes bone marrow transplantation (BMT). This has been shown to be successful in the majority of cases, provided that a fully matched (HLA compatible) sibling (brother or sister) can be identified, and the patient is in a very good condition clinically, i.e. he or she has been receiving appropriate clinical management from the early years. However, only a relatively small percentage of patients (about 20%) will have a fully matched family donor, and considering that this procedure is still an expensive one, BMT cannot be the solution to the total cure of this disease for the majority of patients. BMT for β-thalassaemia is available in Pakistan.
Carrier Status
Laboratory tests for thalassaemia include a routine blood test known as a Complete Blood Count (CBC), which includes measuring the level of haemoglobin and other parameters related to the number and volume of red blood cells, known as Mean corpuscular Volume (MCV) and Mean Corpuscular Haemoglobin (MCH). MCV levels may be lower in children and vary according to age. Red blood cells are also examined under a microscope in order to examine their size and shape. The red blood cells of a thalassaemia carrier will be a paler shade of red and be various shapes (poikitocytosis), compared to normal red blood cells which are a darker red and round and concave in shape.
Tests to determine the presence of the β -trait and confirm that the individual is a carrier of β -thalassaemia include a laboratory process known as haemoglobin electrophoresis, which enables quantitative measurement of haemoglobin. Other haemoglobins normally present in adult red blood cells such as foetal haemoglobin (HbF) may also be measured by electrophoresis. In most cases, the above tests are sufficient to determine whether an individual is a carrier or not.
In some circumstances, genetic or DNA tests need to be carried out in order to confirm whether one is a carrier. Such genetic tests are beginning to be more and more widely used to test for the thalassaemia trait.
Screening should be considered when a relative is known to be a carrier or a thalassaemia patient. Moreover, people who are anemic and do not respond to iron treatment should also have their carrier status donetum orci ultrices non.
Prenatal Diagnosis
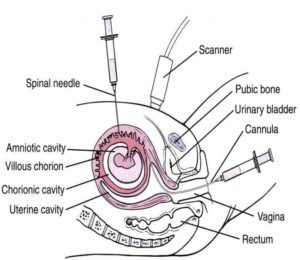
The birth of Beta Thalassaemia major child can be prevented. Couples who are aware that they are carriers of β-thalassaemia, may undergo prenatal diagnosis (Amniocentesis, Cordocentesis and Chorionic Villus Sampling (CVS) to prevent the birth of an affected child. The prenatal diagnosis methiod used in Pakistan is Chorionic Villus Sampling (CVS):
Chorionic villus sampling (CVS) is a test done during early pregnancy to see if the child is affected or not. Chorionic Villi are tiny finger-shaped growths found in the placenta. The genetic material in chorionic villus cells is the same as that in the baby’s cells. Using ultrasound as a guide, the specialist obstetrician removes a small sample of cells from the chorionic villi. The cells are removed either with a thin needle inserted through the mother’s abdomen (transabdominal) or a thin catheter inserted through the vagina (transcervical). The cells are then analysed and a diagnosis made.
Chorionic villus sampling can be done earlier in pregnancy (at 10 to 12 weeks). CVS allows the parents to know the health of their baby and make an earlier decision whether to continue or end the pregnancy. Results of CVS usually take less than a week. Risk of miscarriage in CVS is about 0.5 – 1%.
Membership
Full Members
Provisional Members
Associate Members
Honorary Members