INITIAL APPROACH TO ANY PATIENT WITH THALASSAEMIA PRESENTING TO THE EMERGENCY DEPARTMENT
- Admin
- Aug, 29, 2018
- Publications, Research
- No Comments.
- History according to Thalassaemia diary & history of present illness
- Physical examination- A lot of attention should be given to complaints by patients of respiratory difficulty, extreme weakness, persistent vomiting, palpitation & difficulty in breathing due to walking.
During examination, the following vitals are very important
In case of complication (s) Inform a specialist or a Thalassaemia center as soon as possible.
Insert cannula or IV line
· Labs/ Obtain sufficient samples for
o FBC & differential (nucleated RBC increase “white” count in Thalassaemia).
o Blood Group extended phenotype or cross match.
o Chemistry BUN, Creatinin , electrolytes Na K HCO3 Cl including calcium, LFTs blood glucose, TSH if necessary
o Urine analysis for sugar, protein, haemolysis (chelation can give red urine)
Blood Pressure, Heart Rate
Temperature, Respiratory Rate
Glucose check
Pulse Oximetry
Cardiac Monitor& ECG
STABLE?
| Yes | No |
| Place in appropriate cubicle for observation, investigation | Resuscitate |
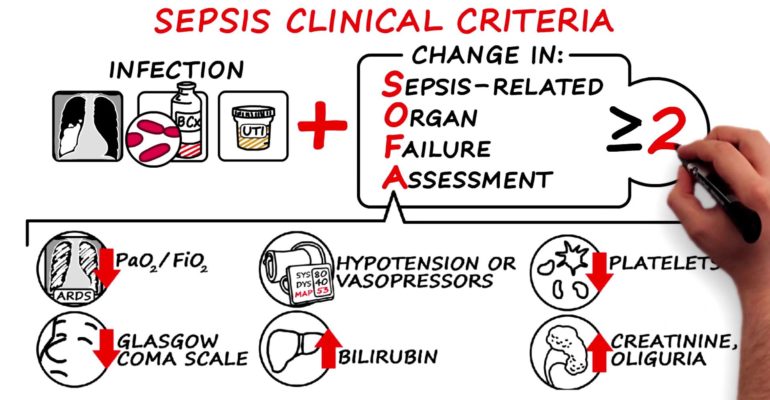
Sepsis
Consider possible causes and investigations.
- Infections are typically bacterial and are often rapidly progressive and potentially fatal.
- Infections are the second cause of death in Thalassaemia Majors, after cardiac complications.
- Thalassaemia patients should be treated as immune compromised if they have a fever.
Common organisms involved include:
- Klebsiella, which may cause septicaemia and shock
- A variety of other gram negative organisms
- Cerebral abscesses.
- Yersinia enterocolitica, more commonly occurring in patients on desferrioxamin. Presents with fever, abdominal pain, diarrhea lymphadenopathy. May mimic acute appendicitis. Difficult to detect and the microbiology laboratory must be alerted to this possibility when receiving samples of stool or blood.
- A variety of gram positive encapsulated organisms may cause infection, particularly in splenectomised patients.
Common foci of infection include:
- Renal tract – UTI, renal stones , renal failure
- Respiratory tract , ARI , pneumonia , tuberculosis
- Abdomen , gasteroenteritis , food poisoning , dysentry
- Cholecystitis
- Colitis, appendicitis (but consider first excluding yersinia)
- Skin infections , osteomyelitis
- Indwelling lines/catheters
- Cerebral (abscess)
- Heart (myocarditis and endocarditis) any infection in the body will decompensate the heart
- Septicaemia without a focus – consider splenectomy and severe iron load.
Treatment
Initial
Normal saline or Ringers lactate 20ml/kg in 30 min then shift to appropriate solution according to age
If gastroenteritis in Paediatric age group, follow WHO plan C
Adult patients alternating normal saline with D/W 5% can be used
Administer blood if Anemic
Give O2 if in distress
- Provide early fluids (avoid overload since many patients have cardiac involvement due to iron toxicity – each case must be assessed according to cardiac status).
- Administer early antibiotics.
- Giving Antibiotic within 30 minutes, significantly reduces mortalitys
- Where affordable give Ceftriaxone or Ampicillin plus Gentimycin in high doses
- In older children and adults I/V Ciprofloxacin can be used
- When giving antibiotics in the emergency unit to a Thalassaemia patient, care should be taken to always cover for penumococci, Haemophilus influenza and Meningococci if splenectomised.
- Acute septacaemia patients should be covered for a range of gram negative pathogens including Klebsiella (ciprofloxacillin is often effective
- Should Yersinia – an intracellular organisim – be suspected, ciprofloxacillin or trimethoprin are usually effective
- Monitoring
- Pulse rate and volumue , mean arterial pressure, if possible
- Provide inotropic agents Dopamin , Dobutamin if indicated.
If a patient has a fever always admit, unless you are advised by the treating Thalassaemia specialist that there is no need to do so.
Membership
Full Members
Provisional Members
Associate Members
Honorary Members